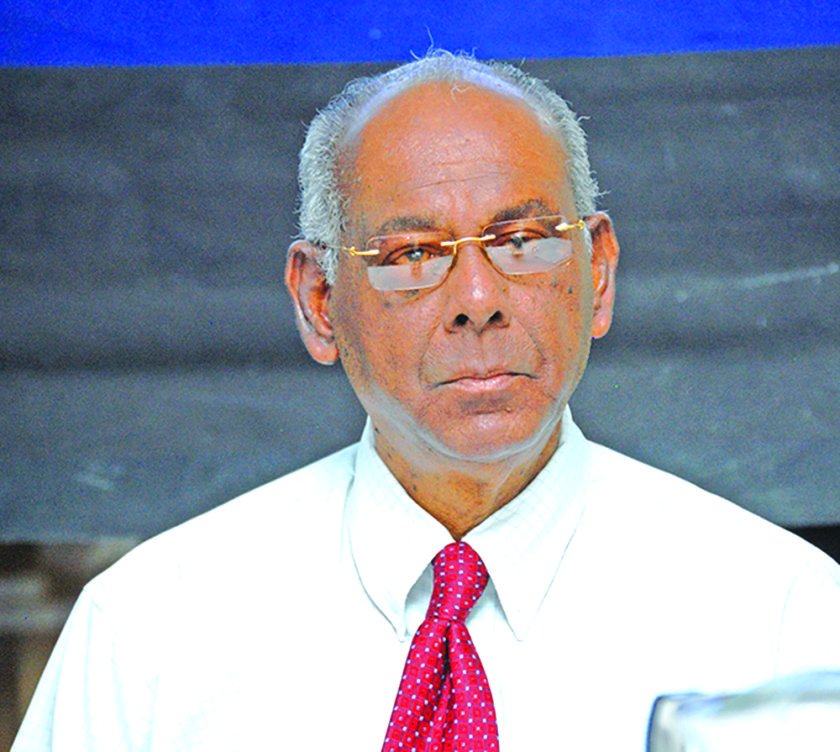
…Says Hospital’s CEO
Linden Hospital Complex (LHC) Chief Executive Officer (CEO), Dr Farouk Riyasat has noted that 41-year-old Jennifer Gill, who died on Monday following a normal delivery at the medical institution, suffered a blood disorder, referred to as Disseminated Intravascular Coagulation (DIC), which caused rapid blood loss and thinning eventually leading to shock and kidney failure.
The CEO made the revelation, which he stated was his belief, during a media brief that was also attended by the Hospital’s Chief Medical Officer (CMO), Dr Romesa McDonald and Public Relations Officer Toshanna Alicock on Wednesday.
Alicock said the institution was saddened by the incident and expressed sympathy to Gill’s family, noting that the Hospital would have completed its investigation and an official report was already prepared and sent to the relevant authorities, including the Chief Medical Officer (CMO) and the Director of Regional Health Services.

She said a Pathologist from Georgetown travelled to Linden on Wednesday to conduct a post-mortem examination on the body of the now deceased woman; however, her family did not show up despite being informed. This led to the procedure being postponed.
Alicock said according to facts from the report, on first assessment by a doctor, Gill was in active labour when she arrived at the Hospital, being dilated at six centimetres (cm) and did not require a C-section.
“On assessment by the consultant, the patient had no criteria for a C- section…,” she noted. Alicock explained that Gill delivered a healthy baby boy and received the necessary drugs and blood that were needed.
“After the patient gave birth, the patient was observed to be haemorrhaging and the patient was then prepped and taken to the theatre to have a hysterectomy.”
She added that Gill went into hypovolemic shock (also referred to as haemorrhagic shock) and was transferred to the Intensive Care Unit (ICU), where treatment was continued.
However, she went into cardio-respiratory arrest, and despite resuscitation, she died at 20:30h on Monday. Alicock maintains that Gill was treated by a team of expert doctors and that immediate family members were kept up to date on her condition by Dr McDonald and other members of the team throughout the process.
The CEO noted that the Hospital provided for doctors to be on call 24/7, refuting allegations that there was no doctor available. He said only the anaesthetic consultant was later called in, but an obstetrician had been present with the patient at all times. An obstetrician was the one to decide if Gill needed a C-section, but he said Gill was found to be in the position to facilitate a normal delivery.
Dr Riyasat reiterated that doctors were on site while consultants were always on call and theatre staff were always available. He added that a doctor was on site when Gill arrived and had observed that she was in labour.
He said the consultant who was called in arrived and did another assessment and Gill was fully dilated by then. Following the normal delivery, Dr Riyasat said, Gill was doing well until about half an hour later when nurses noticed she was bleeding heavily.
He said she was seen by a specialist who did routine procedures and the bleeding stopped but recommenced. Dr Riyasat explained that Gill’s uterus was not contracting despite treatment and doctors made a decision to remove it via hysterectomy. At this time, he said, she was stable and conscious. After the anaesthetic doctor arrived, Gill was taken to the operating theatre.
“Because of the blood disorder that this girl was suffering from, during the surgery, she went into a shock…because the clotting factors were not present within her bloodstream, it wasn’t clotting the blood as fast as she was bleeding … therefore, she end up with DIC, a coagulation disorder – Disseminated Intravascular Coagulation … so … the blood gets thinner…” This, he said, leads to kidney shutdown, but he said Gill was treated for the blood-clotting issue.
Dr Riyasat added that following the hysterectomy, Gill was not passing any urine and died as a result of kidney failure due to rapid blood loss.
According to the CEO, a C-section would have also been life-threatening with the blood disorder, which was only detected after the hysterectomy. He said staff also learnt that a family member of Gill also suffered from the disorder and had to have her uterus removed.
Additionally, he said they learnt that Gill, who had two other children, also suffered severe haemorrhaging during one of her other pregnancies. The CEO said staff only learnt this later, as he explained that specific tests were required to detect the disorder. Prior to this incident, the LHC recorded zero maternal deaths since 2009.